Our childhood might be less important for our lifespans than we previously thought

A decline in serious childhood infections could explain why lifespan has increased. Image: REUTERS/Darren Staples
The Great Exhibition of 1851, housed in London’s Crystal Palace, showcased the newest of culture and science – including the world’s largest diamond, a precursor to the fax machine and barometer which worked entirely through leeches. Living conditions were tough, but having survived to the age of 20, a young Londoner attending the exhibition could expect to live until around 60. A century and a half later, 20-year-old Londoners watching the Olympics down the pub can expect to live to the age of 80.
But what is behind this extraordinary 50% increase in human lifespan since the 1850s? Many factors are at play, including the development of contraception, vaccination, antibiotics and improved nutrition and hygiene. But the impact of each factor has remained a bit of a mystery. This is a shame, as understanding the precise nature of forces behind lifespan is essential if we want to be able to predict how long we may live in the future. To shed some light on this, we investigated church records from Finnish individuals born between 1751 and 1850, just before this huge extension in lifespan, to work out how childhood diseases may affect a population’s lifespan.

As long ago as 1934, a study reported that a person’s chances of dying were determined not by the current year, but by the year in which they were born. The authors of this early study concluded that “the figures behave as if the expectation of life was determined by the conditions which existed during the child’s earlier years”. So what might these conditions be?
In 2004 a new paper put forward a compelling hypothesis to explain the link between early-life conditions and adult mortality. Infectious diseases are caused by bacteria and viruses, which elicit inflammatory immune responses. Many, or severe, infections can lead to chronic inflammation, which is linked to atherosclerosis, a hardening of the arteries, and thrombosis, coagulation of the blood, which are risk factors for cardiovascular disease and stroke. Since 1850, serious childhood infections such as smallpox and whooping cough have largely been eradicated by vaccination and hygiene in industrialised countries.
A decline in serious childhood infections could therefore explain why lifespan has increased: fewer chronic infections, lower inflammation, and less atherosclerosis could have lead to a later onset of cardiovascular disease and therefore longer lifespan.
There is evidence that chronic infections in early life can have a long-lasting impact on inflammation. Union Army soldiers who suffered tuberculosis as young adults during the American Civil War had a 20% increase in risk of cardiovascular disease in middle age. Meanwhile, Tsimane forager farmers in the Bolivian Amazon who live with endemic parasite infections from early life have far higher levels of inflammation than people in the modern US. Despite this link, higher inflammation in the Tsimane does not lead to cardiovascular disease: they are protected by their excellent diet and active lifestyle. This suggests that such diseases are a result of modern lifestyles and may have been rare during human history.
But this is not the whole story. Intriguingly, people in the Ecuadorian Amazon, who also live with endemic infections, seem to have lower levels of inflammation than people in the modern US. This suggests that the experience of infections in early life may alter inflammatory responses in later life and prevent overzealous inflammation.
There is abundant evidence that high death rates in early life are linked to higher mortality in later life. Most such studies use data from pre-industrial populations, because an unfortunate drawback of studying modern people is that they tend to outlive the researchers. In these populations people born in years where the infant mortality rate is higher are consistently shown to have a higher mortality rate as adults.
There is, however, one issue with these findings. Infant mortality has decreased over time. So has adult lifespan. We assume a causal relationship between the two, but the link could be caused by something else, related to both of these, also changing across time.
For example, general improvements in living conditions could drive down infant mortality, through reduced infections, and increase adult lifespan, through improved diet. The link between reduced infant mortality and longer adult lifespan could therefore arise because of improvements in living conditions. To deal with this problem, a statistical technique called “de-trending” is used, so that the data provide information on infant mortality relative to the prevailing conditions.
Lessons from pre-industrial Finland
Using this technique, recent studies have found negligible associations between infant mortality rate and later-life mortality risk. Something missing from these studies, however, is data on disease in early life: infant mortality rate is used as a proxy, but infant death could be related to other factors.
Recently, we used data from church records on death rates from infections in pre-industrial Finnish people. These records contain information about births, marriage, and death for thousands of people. From the death data, we could determine, in every year, what percentage of the children died from an infection. We assumed that lots of deaths meant lots of the surviving children were infected.
We used the “de-trending technique” to remove the change in child disease across time and studied how child infection exposure during the first five years of life influenced later life survival, cause of death, and fertility. The results were very clear: we found no link between infant disease exposure and later-life mortality, death from cardiovascular disease, or later-life fertility. Indeed, the evidence seems to be mounting that the link between early disease and adult lifespan is relatively weak. Similarly, the evidence that people in populations who experience frequent infections can moderate their inflammatory responses also weakens the link between infection and chronic inflammation.
Without a doubt, the fact that modern Londoners generally get enough food, have clean drinking water and access to free medical care will extend their lifespan. Current evidence suggests that these processes acting in adulthood seem to be the dominant factor.
All of this raises the inevitable question: at what point will human lifespan stop increasing? Certainly, every time a prediction is published, it is quickly exceeded. Many researchers agree that as long as living conditions continue to improve, average lifespan could increase for a little while longer, perhaps to the point at which it reaches 100 years. Research into life-extending treatments is exciting both scientifically and commercially, but given we don’t know what may be possible it is hard to predict the limits of human lifespan into the future. But that’s a whole other debate.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Stay up to date:
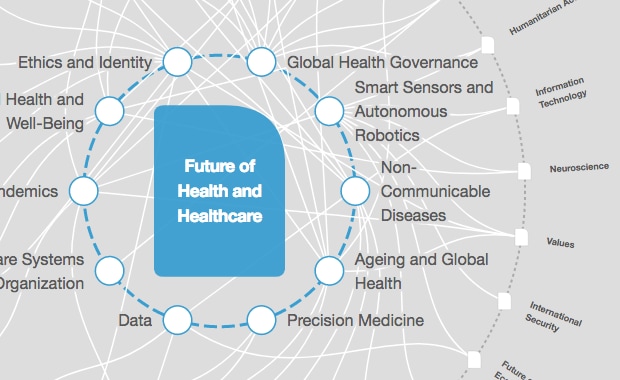
Future of Global Health and Healthcare
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Fernando J. Gómez and Elia Tziambazis
December 20, 2024