What can America learn from Sweden about healthcare?
Access to medical care is just one small part of what makes us healthy
Image: Filip Mroz
Stay up to date:
Healthcare Delivery
“If I have to buy my drugs this month, I won’t have money to eat.”
“Sandy” is a retired senior from South Florida living with diabetes and other multiple chronic conditions. She recently called my company, Humana, to ask us not to ship her drugs because she couldn’t afford them. Sandy was struggling with her diabetes, and her financial situation was making matters worse.
Our call centre representative contacted Humana’s local Florida office for assistance. The office helped address Sandy’s financial needs and arranged for 10 days’ worth of meals to be delivered to Sandy’s home, through an existing programme with a local food bank.
Thankfully, Sandy didn’t have to choose between two things that greatly impact her health. Programmes including Medicare Advantage encourage organizations such as Humana to assist individuals like Sandy beyond their healthcare needs. However, Medicare Advantage programmes are limited within the United States, causing a mismatch between healthcare expenditure and its actual effect on health.
The US spends more than any other country on providing medical services, but access to care is just one small part of what makes us healthy. The underfunding of lifestyle needs impacts healthcare, and is greatly compounded in populations with chronic conditions. (In the US, 75% percent of seniors are living with multiple chronic conditions.)
One example of the variation of US healthcare spending is demonstrated by pharmaceutical spending. The vast difference in expenditures creates a “crowding out effect”. This limits the ability of US federal and state budgets to afford social programmes that can help individuals with lifestyle needs directly associated with health conditions. In some ways, it’s the “chicken and egg” effect.
The US needs to increase its spending on social programmes that decrease healthcare costs. However, it cannot afford to because of the high expenditures from reacting to healthcare problems. This is why it should reallocate some of its healthcare expenditures to programmes that reward for healthier outcomes, rather than just treating the symptoms of bad health.
There is increasing awareness of the impact of social determinants on an individual’s health. Social determinants range in types, but can be classified broadly as the “conditions in the places where people live, learn, work and play (that) affect a wide range of health risks and outcomes”. Social isolation, loneliness, lack of transport and food insecurity are all examples. At Humana,we see firsthand the impact that these social factors have on our members.
Sandy is one of millions of Americans who suffer from food insecurity. Senior citizens are the fastest-growing food insecure population in the US. Research has also shown that seniors who are food insecure are more likely to have higher rates of chronic conditions and other diseases.
So if basic needs like hunger are not being met for Sandy and others, are we spending our healthcare dollars wisely?
According to the OECD database, we’re not. Many other wealthy countries spend about half as much per person on health than the US, yet have better health outcomes and have successfully addressed the social determinants of health.
Consider Sweden. Swedish Commissioner Denny Vagero detailed the country’s unique approach to addressing these health determinants in an interview:
“The Swedish public health policy aims to create the social conditions to ensure good health for everyone. The policy is an outcome of an extended two-decade process of awareness-raising within the health system, and among policy-makers and civil servants in other sectors. The process resulted in a shared understanding that health is not produced by the health system alone. Rather, it is produced by other sectors, and thus is the responsibility of all sectors.”
Sweden’s approach works. Their rate of economic vulnerability is just 4%, while nearly 25% of US seniors often worry about having enough money to buy nutritious meals or pay for necessities such as housing. Only 2% of high-need older adults in Sweden struggle with cost, while in the US it’s 31%. But a holistic approach to health isn’t just about reducing economic vulnerability, it’s about helping people live their best life, and this shows across many dimensions.
Sweden’s integrated healthcare and social policies have helped them rank in the top 10 happiest countries in the 2018 World Happiness Report. Their success with the integrated approach is attributed to their eight focus areas:

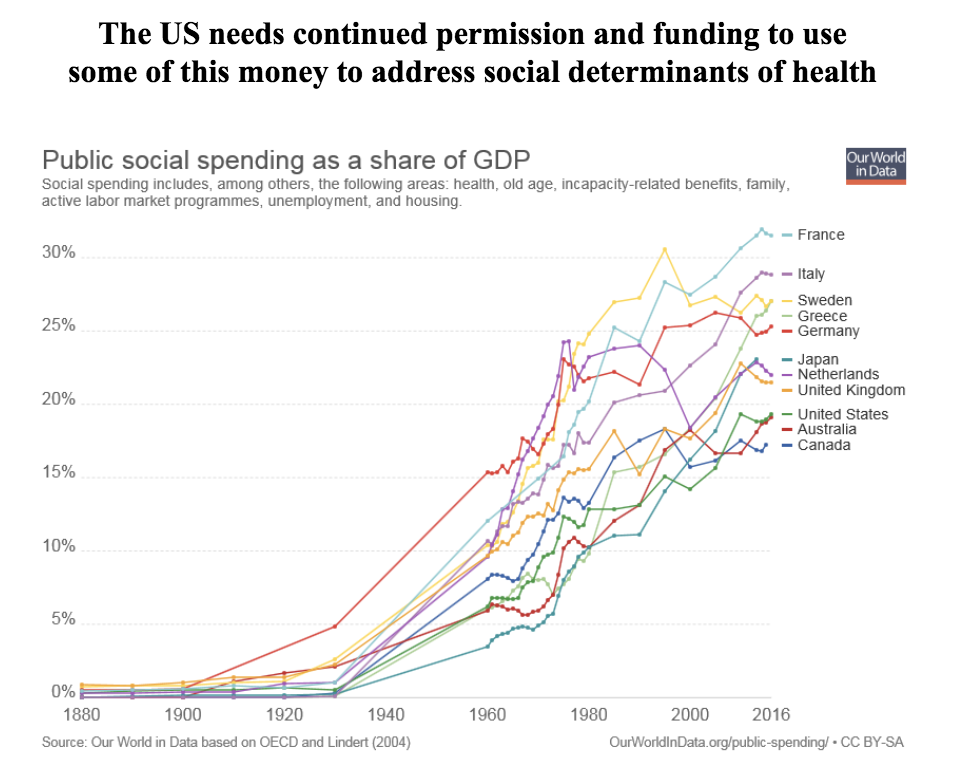
In contrast, the US has traditionally viewed its healthcare system as the primary driver of healthcare and health outcomes. This is changing, as described above, but its spending habits have yet to catch up.
For example, the chart below shows that what the US spends on healthcare alone looks similar to other countries' combined spend on healthcare and social services. However, this is because the US spends less than other countries on non-health social services, although such programmes could indirectly improve health.

When you focus investment on the social determinants of health, you set the foundation for improved health outcomes for the population overall, including seniors.
Yet despite the self-inflicted spending challenges that the US faces today, both federal and state governments are moving in the right direction to improve community health. For example, The Centers for Medicare and Medicaid Services has just started to allow Medicare Advantage plans to include goods such as food and transport.
At Humana, we’re helping 1.5 million seniors living with multiple chronic conditions improve their health and increase preventive care via the Medicare Advantage value-based care reimbursement model. These same seniors are also enhancing their mental and physical health through our Bold Goal initiative. Humana wants to improve the health of the communities it serves by 20% by 2020.
Our Bold Goal experience has taught us that we need to personalize and customize care for each person and address the social determinants of health. We’ve also seen that real change requires partnering in non-traditional ways for collective impact. Community involvement is the foundation, which is why private and government sectors need to work together. Most importantly, these services need to be integrated in a holistic and personalized engagement model for each individual, especially the individuals with fewer resources.
So what lessons can we take from Sweden? The US healthcare industry and government must lead the way by spending healthcare dollars more wisely on the things that influence health, such as its social determinants. If the US does this right, people like Sandy won’t have to choose between food and medicine.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Shyam Bishen
May 27, 2025
Daniella Diaz Cely
May 27, 2025
Silvio Dulinsky
May 23, 2025




