Telemedicine could help the world achieve health equity by bringing care to the home - here's how

Re-centering healthcare to the patient’s home with virtual healthcare tech.
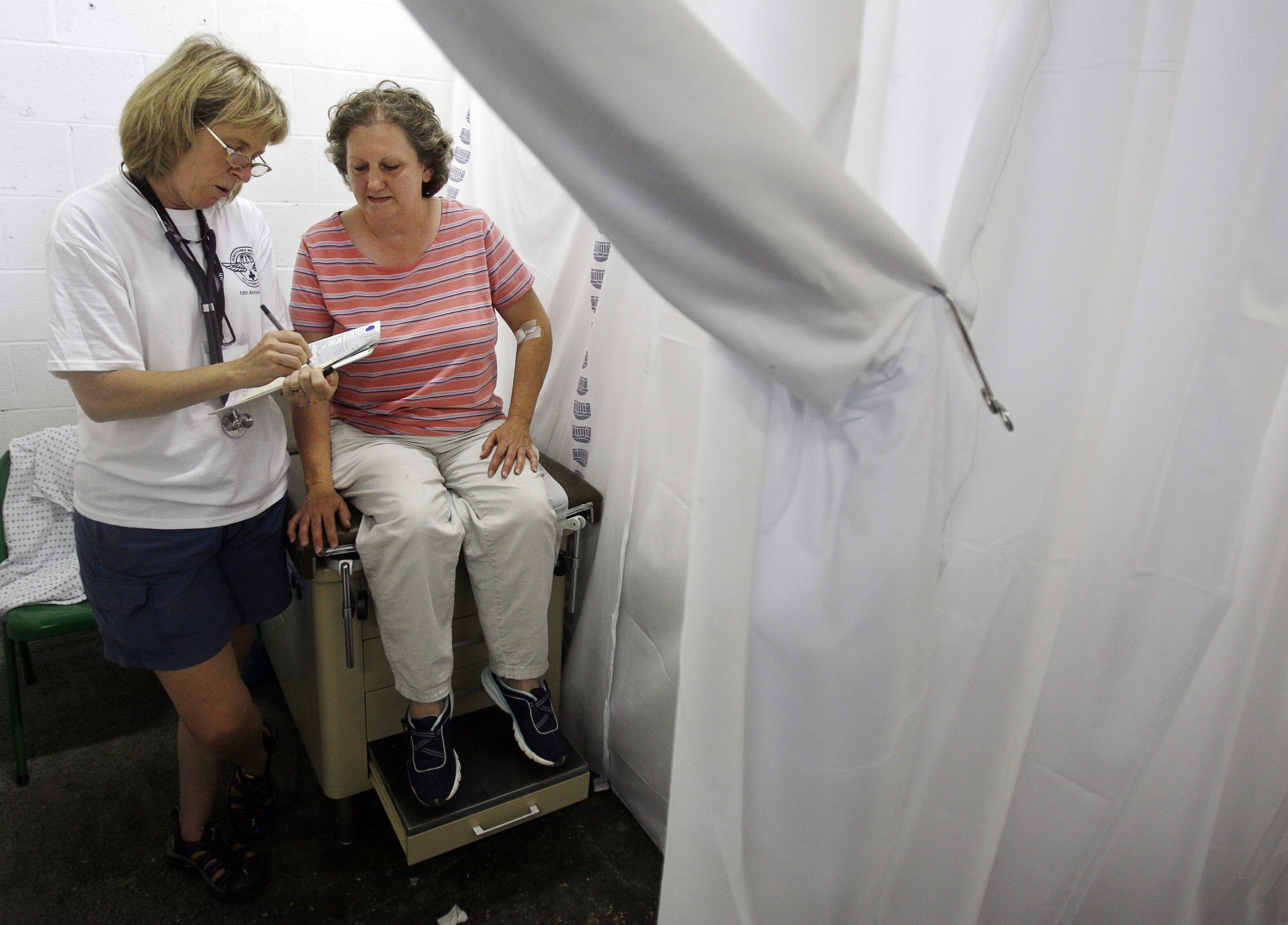
Image: Photo by National Cancer Institute on Unsplash
Stay up to date:
Health and Healthcare
Listen to the article
- Global health equity is yet to be achieved.
- Virtual care technologies, such as telehealth, have the potential to significantly improve global health equity.
- The ultimate result of this predictive and personalized healthcare will be earlier medical interventions that prevent medical crises and lead to better outcomes across countries of all sizes, locations and stages of economic development.
Access to quality healthcare is a global challenge for many reasons. Provider shortages, political instability and economic volatility affect countries of all sizes and stages of economic development. Another major obstacle, which is often overlooked when discussing expanding global health equity, is that many healthcare services are still delivered traditionally through a patient visiting a clinic or hospital, even when an in-person visit is not necessary and could be an obstacle for patients who lack access to care for a variety of reasons.
As the world witnessed during the ongoing COVID-19 pandemic, virtual care technologies, such as telehealth, have opened an enormous care access opportunity for geographies that lack proximity to healthcare professionals.
What is the World Economic Forum doing to improve healthcare systems?
Low-cost remote patient management
When telehealth first came onto the scene as a first-generation iteration of virtual care, millions of people across the world accessed it for the first time. They appreciated how it eliminated the time, expense, out-of-pocket costs and inefficiencies associated with in-person care delivery.
Yet, telehealth is only the beginning of re-centring healthcare to the patient’s home to make it significantly more accessible and affordable. Next-generation technologies, such as remote patient monitoring and management, which include real-time and continuous data collection and analysis from medical-grade biosensors worn in the home, enable clinicians across the globe to address the health inequities and social determinants of health in ways never before possible.
The vast majority (85%) of telehealth patients during the early months of the COVID-19 pandemic lived in high-income countries, likely using wired broadband internet connections. In-home broadband and other high-cost technologies, however, are not always required to effectively implement and grow a tech-enabled remote patient management programme designed to prevent disease exacerbations and associated hospitalisations.
Accept our marketing cookies to access this content.
These cookies are currently disabled in your browser.
The world is ready for virtual medicine
Consider that 95% of the world’s population is covered by a mobile broadband network, according to GSMA Intelligence, and 55% of the population was using mobile internet at the end of 2021. These mobile networks, in most cases, are more than adequate to wirelessly share data with providers many miles away.
Similarly, the average cost of an Internet-of-Things (IoT) wireless sensor decreased by 200% from 2004 to 2018 to 44 cents. And, despite the steep drop in cost, wireless, wearable sensors have significantly improved in performance and features. Consumer-focused smart watches and rings, for example, are built with such sensors, mostly used for tracking exercise activity, sleep and vital signs, such as heart rate.
Medical-grade wearables for clinical purposes have also vastly improved. They can collect dozens of vital signs and novel biomarkers that machine-learning technologies can analyse so that clinicians know what normal looks like for a particular patient. Such sensors have also drastically decreased in price and present an affordable option to expand continuous monitoring of patients within their homes, regardless of their location.
These biosensors, patient biomarkers and other data entered through a smartphone or other mobile device can now automatically flow through existing mobile broadband networks all the way to a healthcare provider’s screen.
Clinician decisions supported through data science
While clinical data is extremely important, analytics must be applied to that data to make it meaningful for the patient’s care team. Providing a tsunami of data to clinicians without that extra step would burden a clinical team that is likely facing staffing shortages and growing demand for care. That is why the third pillar of expanding global health equity is to broadly apply data-science technologies to personalise care and predict outcomes with a high degree of accuracy.
Existing artificial intelligence and machine learning algorithms can compare incoming information against the patient’s health status and history and millions of other comparable patient data points to instantly notify clinicians of a potential health crisis. With this advanced warning — days or even weeks ahead of time — a clinician can intervene through a telehealth or in-person visit and prevent a potential health emergency.
Data science technologies — which 56% of clinicians believe will drive more of their decisions in the future — can also reduce the cognitive burden on providers by offering insight into patients who need care more urgently. Clinicians could then best utilise their years of education, training and experience to prevent a potentially harmful, costly event that further depletes care resources that could be more equitably shared.
Advances in data science, mobile broadband networks and biosensors, combined with the rapid adoption of telehealth and remote patient monitoring, are recognized as a sea change within the healthcare provider community. In 2022, for example, 63% of clinicians worldwide expected most consultations to be conducted remotely in 10 years. In addition, 49% of clinicians agreed the majority of healthcare will be provided in a patient’s home in the next decade.
Effective telemedicine depends on effective collaboration
With provider buy-in and technological support, preventive and chronic condition care in the patient’s home can improve health outcomes and slow cost growth. This approach requires increased cooperation between healthcare providers, patients, government-operated and commercial health insurers, community-based organizations and technology developers. Together, these stakeholders can create a paradigm shift to safely make the home the first option for hospital-level and post-discharge care, as well as chronic condition management.
We will continue to see the expansion of this movement through collaborations that include government, insurers, technology and emerging care providers focused on established tools, as well as newer data science innovations. The ultimate result of this predictive and personalised healthcare will be earlier medical interventions that prevent medical crises and lead to better outcomes across countries of all sizes, locations and stages of economic development.
Have you read?
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Andrea Willige
September 22, 2025
David Elliott
September 22, 2025
Amira Ghouaibi
September 22, 2025
David Elliott
September 19, 2025
Nina Rawal and Dorothy Chou
September 18, 2025
Eric White and Elia Tziambazis
September 18, 2025