5 critical drivers of women and children’s health in under-served rural and refugee communities

Mothers wait with their children for measles vaccinations in Bundung, Gambia. Image: Reuters/Edward McAllister
- Women and children are most affected by healthcare gaps, particularly in a time marked by conflict and climate change.
- Digital technologies, better data and reinforced primary healthcare can all help ensure equitable access.
- Joint action, particularly between public and private stakeholders, will be vital.
During the World Economic Forum Annual Meeting this year, health emerged as a major topic of concern – particularly the health of women and children. The summit saw the launch of the Global Alliance for Women’s Health, a multi-sector global platform backed by 42 organizations and pledges of $55 million. A McKinsey report released the same week revealed a $1 trillion economic gap because of inadequate access to healthcare. Women spend 25% more time in poor health than men, and better women’s health could add $1 trillion to the global economy, with every $1 invested in women’s health leading to $3 in economic growth.
Today, there are increased and intractable humanitarian crises due to conflict and climate disasters. Women and children are most affected, often being forced to flee. In Kenya for instance, 76% of those displaced are women and children, and they have the least access to life-saving healthcare.
To accelerate progress towards health for all by 2030, here are five critical steps to improving access to sustainable maternal and child healthcare, particularly in under-served rural and refugee communities affected by conflict and climate disasters.

1. Achieve long-term viability of health interventions with financing mechanisms leveraging pooled financing for healthcare delivery
In Turkana Country, Kenya, a pilot providing health insurance coverage for children in need of health services including surgery, is currently underway with the support of Rockefeller Foundation. The coverage not only benefits the child, but the whole household. The first surgeries for children as young as five months old were completed this week, and reimbursements for procedures performed will be received in the coming weeks.
This initiative will drive accelerated uptake of health insurance coverage, as community members consider the benefits and make long-term decisions about registering for such protection. This initiative has the potential to strengthen the health system as financing for infrastructure, equipment, supplies and a health workforce is unlocked. This will accelerate progress towards universal health coverage and UN Sustainable Development Goal 3, good health and well-being, by 2030. The necessity of investing in pooled resources to achieve universal health coverage is emphasized by key stakeholders, including the Global Burden of Disease Health Financing Collaborator Network.
2. Roll out new digital technologies with private sector engagement
For example, the Philips Lumify Handheld Ultrasound is a point-of-care system designed to support non-expert users with better-informed decision-making when triaging pregnant women in rural underserved communities. This can help reduce delays in diagnoses and expand access to care by automating image acquisition and interpretation supported by AI. Preliminary evidence from trial interventions supported by the Bill & Melinda Gates Foundation show a positive impact in rural Kenya, where the system has been used to identify abnormalities during pregnancies. In addition, the training time to use ultrasound was reduced from weeks to just hours, which has significant implications for the rapid expansion of the number of frontline health workers who can learn to use the technology and integrate it into routine care. Similarly, a second initiative in north Uganda demonstrated a steady increase in ultrasound skills among nurses and midwives in rural clinics.
For rural and displaced populations with poorer access to health services, these types of digital innovations could be transformational – especially when considering birth defects such as gastroschisis that still have mortality rates approaching 100% in rural sub-Saharan Africa because of delayed diagnoses and lack of surgical care. Investments in infrastructure and equipment can lead to rapid increases in access to care. In Kenya’s Kakuma refugee camp, a 40% increase in pediatric surgical volume was achieved after investments were made in equipment and infrastructure.
3. Ensure that rigorous impact assessments accompany health interventions
Data fosters accountability. Furthermore, data provides critical information for modifying and refining health interventions to maximize and sustain healthcare delivery. It is vital to have both quantitative and qualitative data to have a complete understanding of whether implemented interventions are effective, and what modifications must be made. Economic data is also important to inform governments and policy-makers on which health interventions are cost-effective.
Moreover, contextualized and localized data is critical for effective health interventions and engaging with local governments and ministries of health. Rigorous data can guide and inform policy decisions and governmental actions, help with aligning definitions of success and health indicators, influence policy-making and regulation, while creating accountability. For example, the Digital Connected Care Coalition’s VODAN project is building a locally owned, federated health data infrastructure across nine African countries.
4. Invest in integrated primary healthcare and community health workers to reach the most vulnerable
For UNICEF, improving maternal, child and adolescent health in the most remote, hard-to-reach areas, while preparing for climate change and future pandemics, means investing in integrated primary healthcare (PHC). Central to UNICEF’s approach is empowering community health workers. These individuals – 70% of whom worldwide are women – are the unsung heroes in remote communities. To ensure that women and children around the world have access, UNICEF, alongside public and private actors, launched the Community Health Delivery Partnership (CHDP) at the World Health Summit in October 2023, built on the principles of national ownership, partner alignment and equity.
Critically, the CHDP aims to leverage support and investment for women community health workers, ensuring that they receive the salary, support and supplies they need to deliver vital health and nutrition services. UNICEF-supported community health workers in Pakistan, for example, play a critical role in ensuring a polio-free future by building trust one household at a time. Equitable access to healthcare, especially for the most vulnerable, means supporting the whole health system, including community health workers and the women and children they serve.
5. Ensure health solutions are environmentally sustainable and have minimal carbon footprints
Another critical element to women's and children's health is access to surgery. Two billion children currently lack access to safe surgical care. As we collectively work on improving this situation, we must ensure that this is done with the least impact on the environment; poor environmental conditions invariably lead to poorer health outcomes. Globally, pollution is responsible for at least 9 million premature deaths each year. By innovating together and adopting sustainable procurement practices, we can scale up while reducing healthcare’s carbon footprint and delivering healthcare for all.
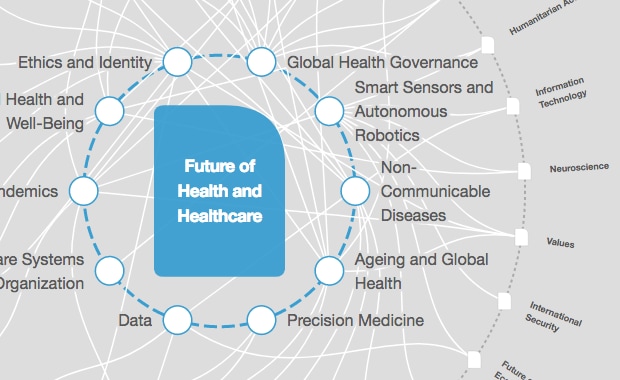
What is the World Economic Forum doing to improve healthcare systems?
Putting these five steps into place, working together as a collective and bringing together resources, expertise and vision, the global health system will be strengthened, accelerating our progress towards health for all. Just six years remain, and the only way we will reach SDG3 in time is through public-private partnerships and joint action. Only by working together can public and private stakeholders, companies, governments, NGOs and peer organizations build the momentum and sense of urgency needed to realize systemic change to deliver equitable and sustainable healthcare.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Stay up to date:
Health and Healthcare
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Judith Love
November 18, 2025