Within 10 years there will be 24 million new cancer sufferers - this is how to care for all them

'We cannot ignore that income inequality and disparities in care fuel cancer’s prevalence'
Image: REUTERS/Omar Sanadiki
Stay up to date:
Healthcare Delivery
- Income equality and disparities in care fuel cancer's prevalence - by 2030 there will be more than 24 million new cancer cases;
- While some countries invest heavily, others under-invest in cancer research relative to the disease burden;
- Access to medical trials for cancer treatments and to the resulting, innovative medicines is not equal across the world.
By 2030, the number of new cancer cases is expected to reach 24.1 million annually. Despite significant progress, cancer continues to steal time that we want to spend with loved ones. It’s the number one killer of working-age adults and costs society billions in lost productivity. Cancer robs us of our most productive years and profoundly impacts the lives of families and caregivers.
We cannot ignore that income inequality and disparities in care fuel cancer’s prevalence. However, I believe that bold approaches and a shared commitment to innovative solutions can alter cancer’s course and ease its burden on both people directly affected and society at large.
Our aspiration is for every person living with cancer to get the treatment they need. Scientific progress means nothing without access to the resulting medicines. With more breakthroughs on the horizon, we must convince governments to treat cancer as a health imperative that is prioritized by healthcare systems with an aim to support market access that rewards true innovation.
Transformative medicines, such as potentially curative CAR-T cell therapies, are an important element in meeting this challenge. However, we must combine these scientific advances with dynamic public-private collaboration.
The path starts with a clear outline of our goals, the obstacles in our way and the levers we have in hand to deliver sustainable cancer care available for all.
Fully embracing value-based care means shifting our focus from “paying per pill” to looking at long-term benefits over a patient’s lifetime – which includes benefits to the patient as well as the healthcare system and society at large. It also means breaking down silos in health system budgets and looking at opportunities to share both costs and savings. This means, for example, that if a medicine reduces post-chemotherapy hospitalizations we allow the flexibility to fund this treatment not just from the pharmacy budget alone, but also by looking at the savings to the hospital budget related to this positive outcome.

I also believe that outcomes-based agreements and indication-based pricing can be part of the solution to get patients the care they urgently need.
The imperative for companies may be to increase resources for educational initiatives to ensure that all stakeholders have a better understanding of innovative payment and reimbursement models that will ensure medicines can get to the patients that need them. Together, we can figure out which payment mechanisms are appropriate given the disease area and population segment.
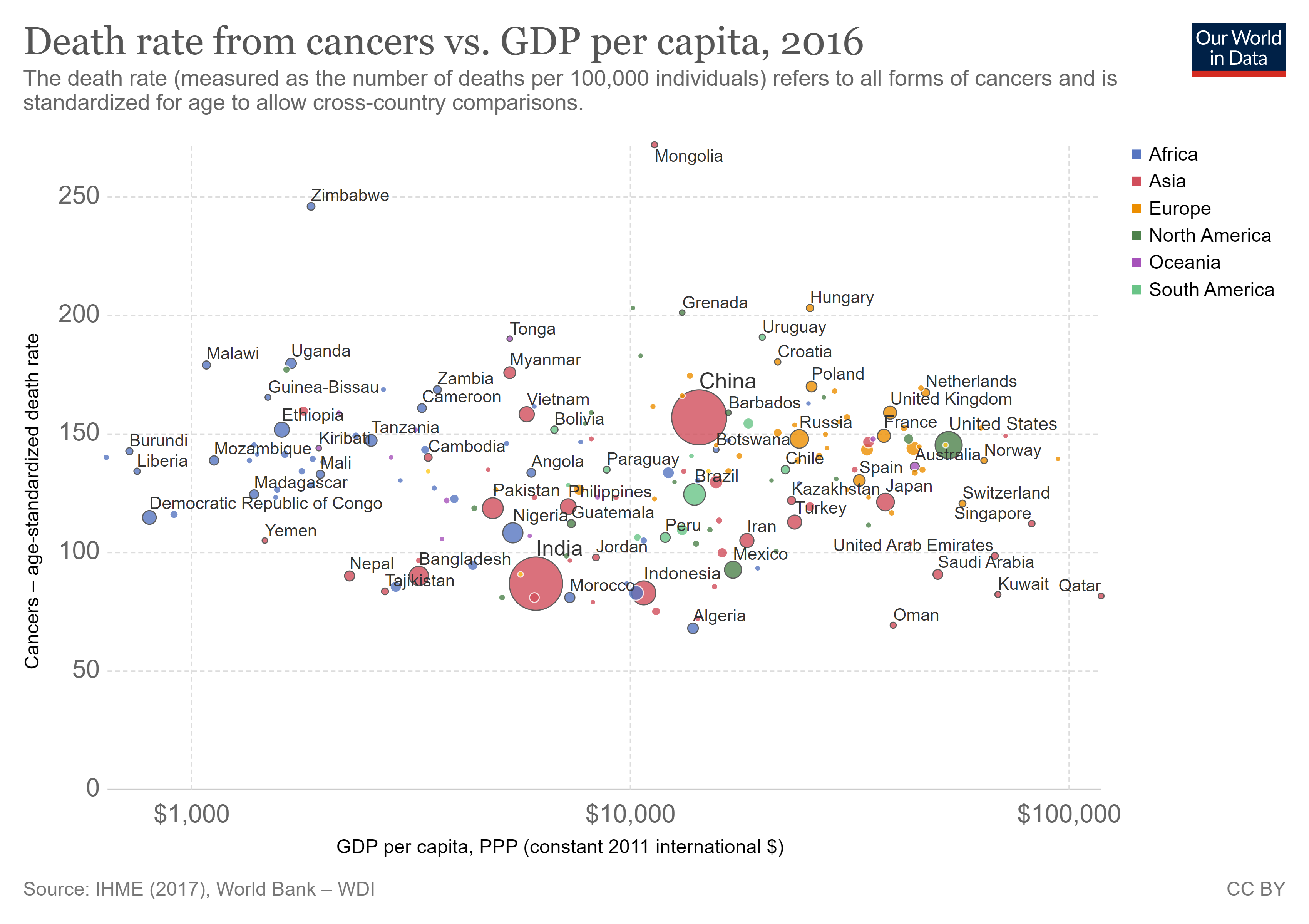
Ultimately, leaders around the world must change how they think and talk about cancer to best serve patients and their families. Across the globe, investment rates in cancer research vary, even among developing nations. While some countries invest heavily, others are underinvesting in cancer relative to the disease burden, which can be higher than heart disease, stroke or dementia. Biopharma plays an important role and this is why we are working with governments, academia and NGOs to encourage greater investment in cancer research and diagnosis.
Despite many government-led efforts to increase racial, ethnic and gender diversity in research studies, progress has been slow in all parts of the world. Access to oncology clinical trials is not equal across the globe. Currently, the median number of trials conducted in high-income countries is more than 100 times the number in low-income countries. Only 8% of cancer patients enrol in trials so removing barriers to entry will greatly help to expand the pool of diverse patient populations participating in oncology clinical trials
Collaboration across borders provides benefits for countries with less trial experience, beyond just providing access to novel medications. As pointed out by the British Journal of Oncology, such studies give local investigators a chance to work with experienced clinical trial organizations while bringing fresh resources to infrastructure and training.
At each stage, this collaboration can help ensure trials advance in a timely manner, reflect diverse populations, and provide access to a wider spectrum of people living with cancer. While obstacles remain, collaborative efforts, such as Cancer Breakthroughs 2020 (formerly known as Cancer Moonshot 2020), have blazed trails.
Partnerships may also be essential to improving cancer diagnoses by putting smarter resources behind testing and analysis. Prevention, early detection and diagnosis are not only critical for life-saving treatment, they can also significantly reduce cost.
In some cases, the problem is reaching remote populations. Breast cancer, for example, disproportionately affects young women in low to mid-income countries. A critical factor is insufficient early detection and the answer does not always lie in more advanced technology. A recent ASCO paper suggests that manual breast examinations may be just as effective as mammography in countries ranging from Malawi to Egypt and Malaysia. If relatively low-tech solutions and education can make a difference in early detection for one type of cancer, the principle may be applicable in many others.
New diagnostic models that do not require the latest technological infrastructure have also been effective in China, where lung cancer mortality has increased by 465% in the past 30 years. In this case, the government worked with municipalities to fund and support multiple cancer screening sites.
With collaboration like this across public and private sectors around the world, we can discover and disseminate good ideas and spread solutions.
A lot is at stake but I have no doubt we will rise to the challenge. I am calling on all stakeholders to work together to ease cancer’s burden on our communities. Together, we can reimagine how cancer is understood, prevented and treated in an equitable manner and alter its course to turn fatal conditions into chronic or even curable diseases.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Naoko Tochibayashi and Mizuho Ota
April 7, 2025
Charlotte Ersboll and Kusum Kali Pal
April 7, 2025
Vivek Vishal
March 31, 2025
Shyam Bishen
March 28, 2025