What is Food is Medicine, and how can it help transform healthcare systems toward more holistic, cost-effective care?

The concept of “Food is Medicine” (FIM) dates back to antiquity, with the writings of Hippocrates emphasizing the deep relationship between food and health.
Image: Unsplash
Dariush Mozaffarian
Distinguished Professor and Jean Mayer Professor of Nutrition, Friedman School of Nutrition Science & Policy, Tufts UniversityStay up to date:
Health and Healthcare
- Food-is-medicine is resurging globally as a viable means to combat chronic conditions and social health determinants.
- Public health reforms and innovative start-ups are playing a key role in driving Food-is-medicine's wider adoption.
- However, significant funding and a paradigm shift is required to make the role of food in holistic healthcare solutions a key feature of societal wellbeing.
The concept of “Food is Medicine” (FIM) dates back to antiquity, with the writings of Hippocrates emphasizing the deep relationship between food and health. However, in scaling global food production to feed a rapidly growing population at the turn of the 20th century, food itself was separated from its connection to health. The reasons for this detachment are manifold, rooted in economic incentives, industrialization, the advent of chemical pesticides, and cultural homogenization, among other trends. The growth of Western medicine, which approached health in a more siloed way compared to Eastern traditions, has also contributed to this bifurcation.
We detail these challenges as well as our strategies for driving multi-stakeholder cooperation in our recently published Insights Report Transforming the Global Food System for Human Health and Resilience.
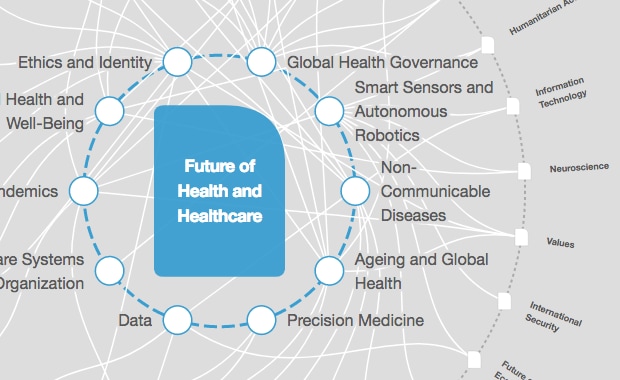
What is the World Economic Forum doing to improve healthcare systems?
As the repercussions of our dietary choices become increasingly apparent, it's imperative to address the root causes of this crisis. Amidst the challenges, the concept of FIM is experiencing a resurgence, driven by several compelling factors. Noteworthy among these are public healthcare reforms, including new “value-based” payer models and the enablement of innovative pilot programs at the US state level to trial nutrition-based interventions. A greater understanding of the social determinants of health, as well as their corresponding societal health disparities, is also driving health systems to consider Food is Medicine interventions. These, along with other trends, are supporting the growth of food-based nutritional interventions to treat diet-sensitive conditions, improve well-being, and advance health equity.
Today, a swath of innovative private sector startups have emerged to address these needs in parallel with community organizations. Funding for FIM startups has witnessed remarkable growth, with $2.5B allocated to startups of the $8 billion in committed private funding from the Biden Administration’s Conference on Hunger, Health, and Nutrition. While the World Economic Forum and its partners are investigating nutrition-forward business models and other opportunities for public-private collaboration outside of the clinical nutrition space, the Food-is-Medicine ecosystem remains the strongest market opportunity to elevate nutrition. We stand on a paradigm shift where food will once again be our medicine.
What is Food is Medicine (FIM)?
FIM represents a solution pathway to resolve several issues. This includes:
- Addressing the prevalence of chronic metabolic conditions, acknowledging the high contribution of nutrition and diet to chronic conditions.
- Tackling the lack of support for social determinants of health, primarily through mitigating the downstream impact of malnutrition/undernourishment on the healthcare system.
- Addressing the dearth of institutional payer support for nutrition insecurity—especially among low-income populations among whom chronic conditions are more prevalent.
- Finally, FIM solutions in tandem with non-traditional payer models address the need for preventative and otherwise holistic care models in a highly fragmented and siloed Western medical system with short-term incentives.
Several trends are now coalescing to support the growth of nutrition-based treatment models. The existing growth in health and wellness has been accelerated post-COVID-19: increasingly informed consumers now have unprecedented access to their health data through wearable technology, AI tools, and digital nutrition and lifestyle tracking technologies.
Additionally, GLP-1 agonist drugs have hit the market, which have yielded substantial behavior changes regarding the volume and mix of foods people eat, with -10.1% Total Packaged Food (-18.8% chips, -15.1% soft drinks, and -11.3% sweet snacks), +46% Fruits and Veggies, and +23% weight-loss foods among clinical trial patients, according to Morgan Stanley. Investors, especially venture capital, now see clear supply and demand signals for healthier eating, allowing them to both support and benefit from the growth of novel, nutrition-based care interventions.
On the public side, demographic changes like an ageing population have supported Food is Medicine as older adults have represented an important proving ground for nutrition-based clinical interventions, among other SDOH’s, through Dual Eligible Special Needs Plans (D-SNPS), among other specialized public-payer plans.
From an executive perspective, the Biden-Harris Administration Conference on Hunger, Health, and Nutrition has created renewed support for FIM in in healthcare, as a political issue, as a business opportunity, and among non-profit and community based organizations, alike.
From a legislative perspective, the Chronic Care Act of 2017/2018 has paved the way for alternative treatments for individuals covered under public programmes who suffer from chronic conditions.
From a regulatory perspective, guidance from the Centre for Medicare and Medicaid Services (CMS), the authority on public payers which operates under the Department of Health and Human Services (HHS), has been transformational in re-aligning incentives to support outcomes through the advent of value-based and other capitated risk payer models.
At the state level, the application and approval of Medicaid “demonstration waivers” have supported individual US states to pilot innovative, nutrition-based FIM interventions.
The USDA, which operates national food assistance programmes like the Supplemental Nutrition Assistance Program (SNAP) among others, has been a valuable vector for FIM through innovative programs like GusNIP, which focuses on nutrition incentives and produce prescriptions in the context of food assistance.
While there has been substantial work to get to this point, greater coordination between public and private players is needed to implement Food is Medicine interventions at scale.
Applications and institutional vectors
While it’s self-evident that nutrition is a causal factor of health status, there is still a gap in research to understand the impact of specific nutrition interventions on patients with complex chronic conditions.
Proving each use case to large payers and institutions to demonstrate health impact, cost-effectiveness, or other positive outcome improvements is crucial for establishing scalability and viability.
These can take the form of elder care, post-discharge care, high-risk pregnancy care, medical nutrition therapy for specific chronic diseases, among other food benefits through certain Medicare Advantage plans’ Special Supplemental Benefits for the Chronically Ill (SSBCI). Several World Economic Forum partners and community members are taking action to close this gap.
Kaiser Permanente, a leading US integrated health care system, has joined forces with the Tufts Food is Medicine Institute to conduct Food is Medicine research across clinical pathways, and with Instacart to expand nutritious food access to its California-based Medicaid patients.
Accenture is currently running a pilot programme to improve health care for vulnerable populations with the goal of supporting health equity. Other non-profit community organizations are also trying to both participate in reimbursement as well as provide meals and food assistance as a charitable good.
Bayer has teamed up with Kroger to provide meals for rural Americans, through Feeding America’s network of community-based organizations. Multi-sectoral partnerships like these will be crucial to support the growth of Food is Medicine.
Remaining challenges
While the promise of FIM is clear, several challenges hinder widespread adoption. The food environment, dietary patterns, cultural practices, as well as other exogenous factors all play a role in what foods we eat.
Thus, implementing a societal philosophy of healthier eating will require a broader change to the default food options and even normative societal behaviour.
On the individual level, long-term behavior change through adherence to diet and lifestyle adjustments remains a key struggle, although one that the direct provision of healthy food through Food is Medicine strategies appears to make more manageable for many patients and providers, alike.
Doctor and other clinician education around nutrition remains lacking. In one large survey, US medical students reported an average of only 5 hours over the 4 years of medical school.
Yet, given the changing paradigm around FIM taking place today, medical nutrition education should be expanded, including potentially through new requirements for accreditation of medical schools and residency and fellowship training programs, and new content on board-certification exams for primary care providers. Indeed, 9 in 10 medical students felt that it was critical to receive formal training on nutrition counseling to optimize patient care.
While nutrition-based clinical interventions have been growing under public-payer programs, there has been minimal adoption among large private payers operating in traditional fee-for-service models without additional metrics tied to quality or value.
Policymakers need to continue to support the growth of innovation in the Food is Medicine space by supporting the gathering and reporting of pilot program data run at the state level, reforming the Farm Bill including its subsidies and nutrition security programs to support healthier eating, expanding Medicare and Medicaid coverage for FIM, RDN counseling, and medical nutrition services, and supporting the continued growth of payer models that support incentives for preventative care, including through nutrition.
Accept our marketing cookies to access this content.
These cookies are currently disabled in your browser.
FIM business models
New business models are evolving to solve the problems associated with the implementation of FIM. The rapid advancement of AI technology, digital tools, and wearable devices also plays a pivotal role in enabling these pathways, through increased scalability but also the data needed for screening and tracking patients.
Some emerging models include:
Integrated clinical nutrition platform providers: Season Health and NourishedRx
- Benefits: offer a one-stop-shop for nutritionist support, education, medically tailored food delivery, and often other health tracking tools.
- Scale: High, these and other integrated solution providers offer a plug-and-play solution for health payers and other institutions and individuals with chronic conditions
- Gaps: Focused on disease management rather than prevention
- Stat: The global medical foods market of $22.4 billion is projected to grow rapidly with the evolution of FIM.
- Benefits: Existing scale (distribution, size, resources), often with captive health units (synergies)
- Applications: Medicare Advantage (and other VBID) partner for grocery benefits (not clinical application-like platforms)
- Scale: Very high existing grocery footprint, with less behaviour change required vs other delivery methods
- Gaps: As MA plans to shift to managed benefits, retailers need to develop their scoring systems to prove they’re not driving up costs without meaningful benefits
- Stat: Annual grocery spending among 48 million households with individuals with chronic diseases in the US: $270 billion in 2022.
- Benefits: US employers’ “double incentive”
- Applications: preventative workforce health, productivity boost and absenteeism reduction
- Scale: Relatively high, given a preventative orientation
- Gaps: health equity – individuals who aren’t employed, are underemployed, or whose employer doesn’t offer these benefits could be left out
- Stat: Some studies show as much as a 50% reduction in absenteeism through consuming a high-quality diet, with positive effects on worker productivity as well.
Sustaining the FIM momentum
The rapidly evolving landscape of FIM not only showcases meaningful potential in transforming the healthcare system toward more holistic, cost-effective care. It also reflects one important solution to the global health crisis caused by the detachment of food from its health-oriented roots and the worldwide growth of unhealthy, ultra-processed foods, which were designed to feed a growing population but are now contributing to the burden of diet-related chronic disease.
The World Economic Forum’s New Frontiers of Nutrition initiative as well as its partners and community members are committed to the growth at the intersection of food and health, capitalizing on public-private partnerships for sustained human health and resilience, with the potential for global expansion.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
David Elliott
September 19, 2025
Nina Rawal and Dorothy Chou
September 18, 2025
Eric White and Elia Tziambazis
September 18, 2025
Jan-Willem Scheijgrond and Syaru Shirley Lin
September 18, 2025
Ashwini Sharan and Abhishek Jain
September 15, 2025